At a Glance
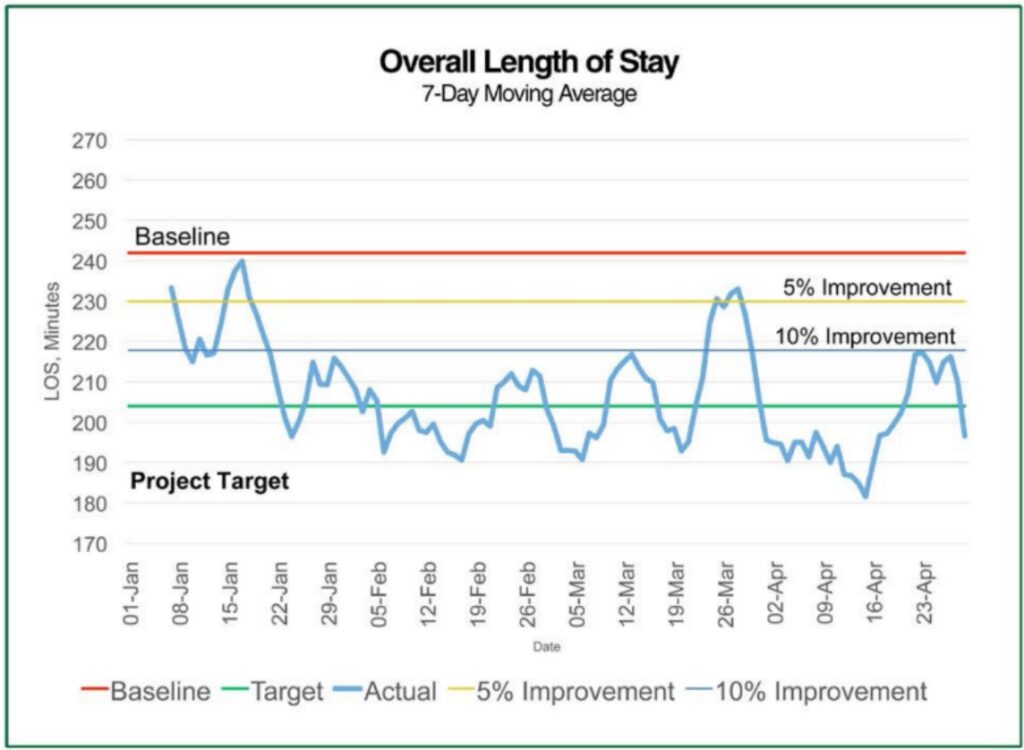
- With an improved performance management process in place, the client reduced the overall length of stay for patients by 18%
- The number of patients who were left without treatment decreased by half
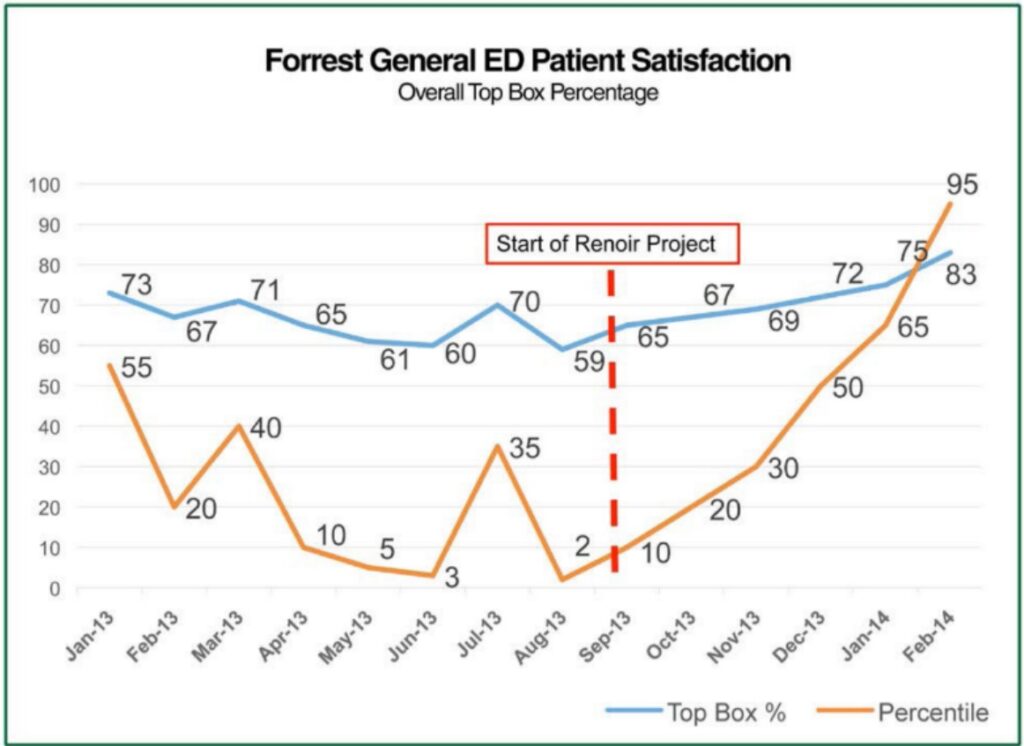
- Patient satisfaction scores rose from 59% to 83% after 32 weeks of project implementation
Background
The client is a general hospital and trauma centre located in Mississippi, US, that provides regional health services. Its Emergency Department contains more than 50 rooms for patients and serves more than 80,000 of them each year.
Analysis
Renoir’s initial analysis determined that issues in the client’s emergency department were mainly in the following areas, all of which had an adverse effect on patient length of stay, patient satisfaction, and staff satisfaction.
Poor Data Accessibility
The operational data produced by the client’s main IT system, EPIC, was not actively used and performance data was difficult to obtain.
Inconsistent Processes Across Departments
Many of the hospital processes lacked consistency across departments and channels of communication were limited, creating inefficiencies and siloes.
Roles and Responsibilities
Staff responsibilities were unclear and did not accurately reflect job descriptions.
Performance Management Processes
Key performance indicators were absent, resulting in a lack of performance reviews.
As a result, patient length of stay and patients left without treatment (LWT) were increasing, and the root causes impacting length of stay were not fully understood. Meanwhile, all this also led to a decline in patient satisfaction scores over the previous two years, as well as staff satisfaction dropping, resulting in a high registered nurse (RN) turnover rate.
Project Approach
Post-analysis, the project was structured into two phases, an 8-week Focus Process® and an implementation phase lasting 32 weeks. During the Focus Process®, four Management Action Teams (MATs) met weekly to identify opportunities for improvement in four key areas that affected the patient’s length of stay, namely entry and admission, patient care and coordination, discharge and admits and support services.
Once the teams identified the top areas for improvement, they concentrated on developing solutions as well as realization plans that incorporated achievable time commitments. Planning, training, compliance, and root cause analysis became the primary focus points of the four MAT teams, which were eventually consolidated into a single team.
Implementation
During the weekly MAT meetings, the client task force, along with the Renoir project manager, delivered presentations to the group regarding KPI performances, key achievements, and any action items raised from the previous week.
Root cause analysis of any issues raised was also discussed during these meetings and suggestions were shared by both Renoir and the MAT for continuous improvement. Action items were then assigned for team members to report back during the following weekly meeting.
By the end of the project, the following solutions had been implemented for streamlined performance management:
- Internal service-level agreements were signed between the ED and support areas for clarity of department roles
- Nursing team SOPs and approach were developed and implemented, and Acuity Training was provided to ensure existing systems like EPIC were fully utilized
- A designated Minor Care fast track for low-risk patients was created to reduce overall length of stay for patients
Key Results
After the 32-week implementation and continuous improvements to performance, the results were as follows:
Average length of stay
↓ 18%
Average Leave Without Treatment (LWT)
↓ 50%
Patient satisfaction scores
↑ to 83%
Registered nurse staff completed acuity training
Optimize your performance management process with the help of our experts.